Dr. David Unwin, a.k.a. @LowCarbGP, is a standout among my Health Sherpas. Over the last 9 years he has revolutionized his National Health Service practice just north of Liverpool, England by encouraging patients with Type 2 diabetes to adopt a low-carbohydrate diet.
More than 100 of these patients have been able to reverse their diabetes and get off their diabetes medications.
Before his low-carb change, he had never seen that happen among his patients.
Not even once.
In the video below, Dr. Unwin shares several of those patient examples, as well as research that supports the assertion of his colleague, Professor Roy Taylor, which is the title of this post and of the video.
Some of Dr. Unwin’s key nuggets:
- Type 2 diabetes, raised triglyceride levels and abnormal liver function are linked to each other and to increased mortality.
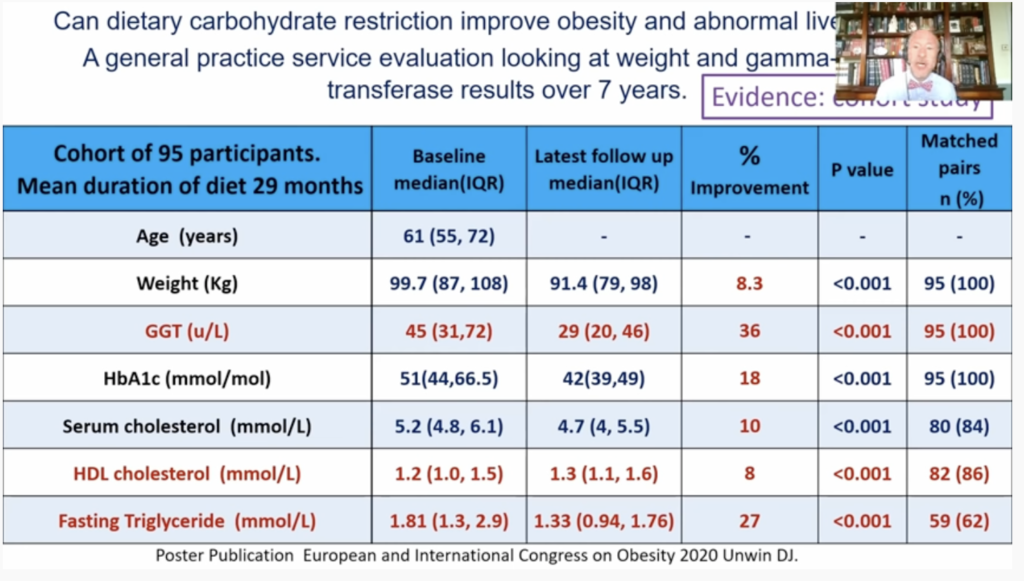
- 24% of the patients in his practice had abnormal liver function (GGT) tests, and 32% had an abnormal triglyceride result.
- For several years he would watch these lab results with a feeling of helplessness because while he knew these patients were at higher risk of both cardiovascular disease and death, he didn’t really know what to do to help them. Statins, which are often prescribed for high cholesterol levels, don’t really help with triglycerides.
- High triglyceride levels and low HDL-cholesterol are strong predictors of a poor outcome with COVID-19.
- 25% of the developed world has Non-alcoholic Fatty Liver Disease.
- 3.3 million people have died of COVID-19 worldwide in the last 18 months. 4.2 million die of diabetes every year.
- He then shows the example of a patient with diabetes, high triglycerides and abnormal liver function, and that cutting carbohydrates fixed all three problems. He also details why this works.
- High carbohydrate diets not only lead to fat accumulation in the liver and pancreas, but even in the tongue, which could be responsible for sleep apnea.
- Many patients with fatty liver are dismayed to be treated with suspicion by their physicians, who believe the patients must be consuming excessive alcohol. In reality, the fatty liver in these patients is due to an excess of carbs.
- Dr. Unwin has developed infographics to help patients identify which foods have high carb loads, and what the equivalent teaspoons of table sugar would be in each.
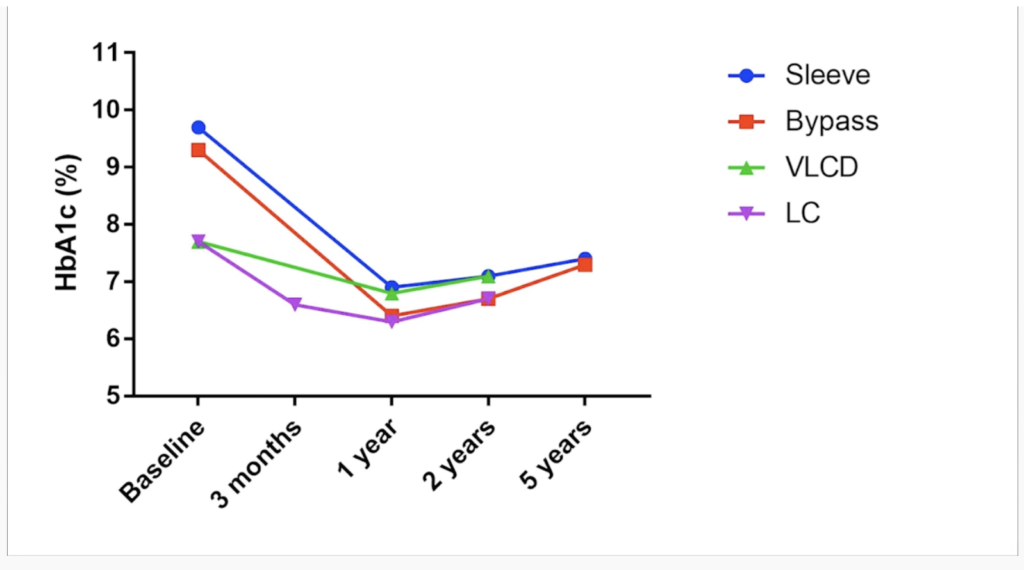
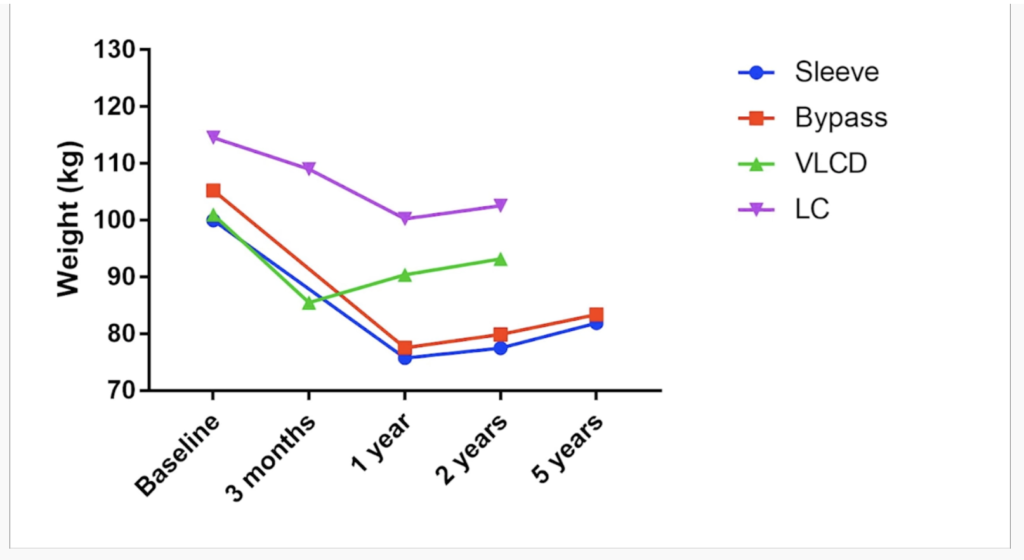
- Finally, he shares compelling data from his practice, showing the improvements in triglycerides, HDL-c, liver function, weight and HbA1c after patients adopt a low-carbohydrate diet.
Dr. Unwin is unfailingly polite and understated in his delivery, which makes his conclusions all the more compelling.
I believe you’ll find this video well worth your time to watch and listen.
For more of his wisdom, see Dr. David Unwin on Cutting Carbs.
Building on our last few years’ experience and the results of our health journey, my wife Lisa and I are launching a new health-related venture next month, working with a friend who is a family physician. He shares Dr. Unwin’s concern about metabolic syndrome and his passion for equipping patients in making diet and lifestyle changes that can dramatically improve their health.
If you’re interested in learning about it, send me an email and I’ll be in touch to give you a preview.